Defining the Core
The “core” goes beyond the abs. It’s a network of muscles that stabilize the body and support posture, including:
• Pelvic Floor Muscles: Support the bladder, uterus, and rectum, and play a key role in bladder control, sexual health, and stability.
• Transverse Abdominis: A deep abdominal muscle that wraps around the torso like a corset, supporting the spine and internal organs.
• Diaphragm: A muscle that separates the chest from the abdominal cavity, essential for breathing and core stability.
• Multifidus: Small muscles along the spine that provide support during movement.
These muscles work together to ensure effective movement and injury prevention.
Understanding the Pelvic Floor
Your pelvic floor consists of muscles and connective tissue forming a support system at the base of the pelvis. Their functions include:
1. Supporting Internal Organs: These muscles support the bladder, uterus, and rectum. Weakness can lead to pelvic organ prolapse, which is more common after vaginal births (Wu et al., 2014).
2. Controlling Bladder and Bowel Functions: Strong pelvic floor muscles prevent urinary incontinence, affecting nearly 50% of postpartum women. Pelvic floor exercises can reduce incontinence by up to 70% (Dumoulin et al., 2018).
3. Enhancing Sexual Function: Strengthening these muscles improves sexual function, with 62% of women reporting better satisfaction after pelvic floor training (Bø & Hilde, 2021).
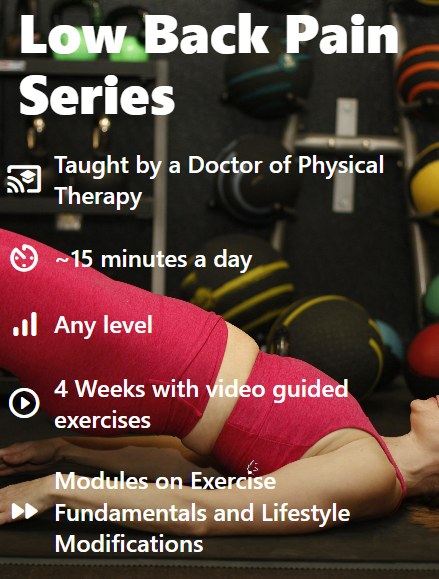
4. Promoting Core Stability: As part of the core system, a strong pelvic floor enhances stability and can reduce lower back pain, which affects nearly 80% of postpartum women (Ostgaard et al., 1991).
Common Issues Women Face
After childbirth, many women experience pelvic floor dysfunction, including:
• Urinary Incontinence: Involuntary leakage of urine, affecting 25-45% of postpartum women.
• Pelvic Organ Prolapse: The descent of organs due to weakened pelvic muscles, occurring in 1 in 5 to 1 in 2 women, with increased rates over age 50.
• Pelvic Pain: Chronic pelvic pain can disrupt daily life and affects around 20% of postpartum women (Nikolajsen et al., 1997).
Recognizing these symptoms early helps prevent long-term complications.
The Importance of Core and Pelvic Floor Health
The core and pelvic floor work together, making strengthening both essential for postpartum recovery. Pelvic floor training reduces incontinence by 50-70%, while reintroducing diaphragmatic breathing can improve pelvic floor health and core stability by 20-30% (Selman et al., 2022).
Pelvic Floor Myths and Misconceptions
Misunderstandings about pelvic floor health are common:
• Myth: Kegels are the only way to strengthen the pelvic floor.
Reality: Kegels aren’t for everyone. The pelvic floor engages reflexively during activity, and training it to do so is key. About 30-40% of women perform Kegels incorrectly (Bø et al., 2007).
• Myth: Only women with incontinence need pelvic floor exercises.
Reality: All women can benefit from understanding and strengthening their pelvic floor.
• Myth: Pelvic floor exercises only involve contractions.
Reality: Rehabilitation involves both contraction and relaxation, teaching the pelvic floor to engage naturally during movement.
Key Exercises to Reconnect
Here are foundational exercises to strengthen the core and pelvic floor:
1. Diaphragmatic Breathing:
• Lie on your back, knees bent.
• Place one hand on your chest, one on your abdomen.
• Inhale through your nose, feeling your abdomen rise.
• Exhale, gently engaging your pelvic floor. Repeat for several minutes.

2. Pelvic Tilts:
• Lie on your back with knees bent or get on hands and knees.
• Inhale, then exhale as you gently tilt your pelvis, engaging your pelvic floor. Hold and release. Repeat 10-15 times.

3. Bridge Exercise:
• Lie on your back, knees bent.
• Inhale, engaging your pelvic floor.
• Exhale as you lift your hips, creating a straight line from shoulders to knees. Hold, lower, and repeat.

4. Tuning Into Your Pelvic Floor:
• Imagine stopping the flow of urine to locate your pelvic floor muscles.
• As you exhale, gently engage the pelvic floor while sitting. Repeat 4-5 times.
Integrating Core and Pelvic Floor Work into Daily Life
To make core and pelvic floor exercises easier to fit into your day, try these practical tips:
1. Pair with Daily Activities: Do exercises while feeding, changing diapers, or sitting.
2. Maintain Good Posture: Stand and sit tall to support pelvic alignment and reduce strain.
3. Avoid Heavy Lifting: Engage your core and pelvic floor while bending your knees when lifting.
4. Stay Active: Gentle activities like walking or yoga promote pelvic health and recovery.
5. Listen to Your Body: Seek help from a pelvic health physical therapist if you feel discomfort or symptoms of dysfunction.
Conclusion
Understanding the connection between your core and pelvic floor is key to postpartum recovery. By incorporating mindful exercises and good posture into your routine, you’ll support your recovery and set yourself up for long-term health. Prioritizing these areas will help you regain control over your body and enhance your well-being.
Take-Home Points:
1. Know your core: It’s a system that includes pelvic floor muscles, the diaphragm, and deep abdominal muscles.
2. Pelvic floor importance: These muscles support organs and help with bladder control, sexual function, and stability.
3. Common challenges: Postpartum women often experience incontinence, prolapse, or pelvic pain.
4. Reconnect with key exercises: Diaphragmatic breathing, pelvic tilts, and bridges help restore strength.
5. Practice in daily life: Incorporate exercises into routines and maintain good posture to ease recovery.
References
• Bø, K., & Hilde, G. (2021). Pelvic floor muscle training: A systematic review. Neurourology and Urodynamics, 40(7), 1787-1795.
• Cohen, S. L., et al. (2021). A systematic review of pelvic floor muscle training for pelvic floor dysfunction. Obstetrics and Gynecology, 138(4), 604-610.
• Dumoulin, C., & Hay-Smith, E. J. C. (2015). Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database of Systematic Reviews, (5), CD005654.
• Dumoulin, C., et al. (2018). Pelvic floor muscle training for urinary incontinence in women: A systematic review. Neurourology and Urodynamics, 37(1), 89-94.
• Wu, J. M., et al. (2014). Prevalence and incidence of pelvic floor disorders in U.S. women: Results from the National Health and Nutrition Examination Survey. Obstetrics and Gynecology, 123(6), 1201-1206.
• Selman, J. R., et al. (2022). The role of diaphragmatic breathing in postpartum recovery: Implications for rehabilitation. Journal of Women’s Health Physical Therapy, 46(2), 85-92.
• Thom, D. H. (2021). Urinary incontinence: The silent epidemic in postpartum women. Journal of Maternal-Fetal & Neonatal Medicine, 34(6), 849-855.